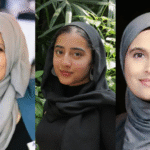
GAZA COMMUNITY MENTAL HEALTH PROGRAM STAFF PROVIDING PSYCHOLOGICAL SUPPORT TO DISPLACED CHILDREN, WOMEN, ELDERLY PEOPLE, AND PEOPLE WITH SPECIAL NEEDS IN EVACUATION CAMPS IN DEIR AL-BALAH AND RAFAH, IN MARCH 2024. (PHOTO: GAZA COMMUNITY MENTAL HEALTH PROGRAM/FACEBOOK)
Gaza Community Mental Health Program (GCMHP) is a non-profit organization offering primary, secondary, and tertiary mental health interventions in the Gaza Strip since 1991. Despite the complete devastation of its Gaza headquarters in Khan Younis and the evacuation of its Deir al-Balah office due to severe damage, the organization remains committed to its mission.
Following the recent incursion of Rafah, the team at the temporary base evacuated the place, and almost all of them got displaced again. This has resulted in the organization being left with just one operational temporary base in Deir Al-Balah.
The organization faces grave challenges imposed by severe war conditions, including the destruction of its premises, staff dispersal, communication breakdowns with patients, and the depletion of medications, it has established temporary bases to provide essential mental health services in Deir al-Balah and Rafah.
Mental health professionals themselves are part of the Palestinian population, with many experiencing loss, displacement, or grief. Despite the overwhelming odds, they persist, their dedication unwavering even as resources dwindle and challenges multiply.
The organization continues to provide specialized psychosocial support sessions for its medical workforce before they engage with patients. These sessions, whether individual or group, help employees alleviate the psychological pressures they face. In its temporary headquarters in Deir al-Balah, about 35 employees work, including administrators and professionals– psychiatrists and psychologists.
Treatment amid turmoil
The prolonged and devastating war, coupled with frequent communication disruptions, has hindered patients’ access to the organization. “Our patients try to reach us but cannot. Either because they are in dangerous locations or due to transportation difficulties. Many lack the financial and physical means to do so,” Dr. Amal Abu Obada, a psychiatrist at GCMHP, told Mondoweiss.
GCMHP used to receive thousands of patients of all ages at its three locations. Some of its teams conduct field visits to reach patients who have difficulty accessing the center for care.
Despite space constraints and increasing demand with daily referrals for new cases, the program strives to provide medical and/or behavioral therapy for about 25 patients daily at its temporary base.
The war has exacerbated the suffering of mental health patients and increased the complications of their conditions. Sleep difficulties, anxiety, psychotic disorders, and depression, have worsened under the harsh war conditions and spread among victims of loss, displacement, and trauma.
Though both treatments are vital, psychiatric patients rely more on medication than behavioral therapy. With the increasing number of patients needing regular medications, especially those with chronic mental illnesses, demand for psychiatric drugs has surged.
Like any medical establishment in Gaza, GCMHCP faces a severe shortage of essential medications, forcing them to resort to alternatives. “We received the latest two batches of medication through WHO. But they are insufficient. In psychiatric treatment, it is preferable to continue with the same medication that has shown improvement, but unfortunately, we are forced to use alternatives that are not as effective,” Dr. Abu Obada explained.
The depletion of all types of psychiatric medications and the use of substitutes have negative effects on patients, including increased symptom severity, complications, and acute relapses. The two temporary bases have only been operating for four months, before which, many patients have discontinued their treatments, leading to severe relapses and complications.
Contact remains severed with many patients, and their fate remains unknown.
Accessing care in crisis
The difficult conditions patients face increase the suffering of their caregivers. Patients require containment and social support, especially those with psychotic disorders like schizophrenia. In the absence of medication and behavioral therapy, patients with such disorders experience severe nervous breakdowns, which can lead to self-harm and harm to others.
With families in overcrowded displacement areas along with inadequate societal awareness to handle such relapses, the load on caregivers to help and alleviate their patients’ suffering increases.
Meanwhile, families themselves undertake challenging daily tasks, requiring significant time and effort to provide basic necessities for their members, not to mention the intense psychological pressures they grapple with.
Dr. Abu Obada recounted the story of one such patient. “A woman wept to me: ‘My son hurt me, Doctor. He never did. My son has been off treatment for two months. I’ve been trying to contact anyone, but I couldn’t reach any.’” Dr. Abu Obada also explained how internet and communication cuts also contributed to contact being severed with a large number of patients, many of whom are now unaware of the new temporary locations and services.

Despite space constraints and increasing demand with daily referrals for new cases, the program strives to provide medical and/or behavioral therapy for about 25 patients daily at its temporary base.
The war has exacerbated the suffering of mental health patients and increased the complications of their conditions. Sleep difficulties, anxiety, psychotic disorders, and depression, have worsened under the harsh war conditions and spread among victims of loss, displacement, and trauma.
Though both treatments are vital, psychiatric patients rely more on medication than behavioral therapy. With the increasing number of patients needing regular medications, especially those with chronic mental illnesses, demand for psychiatric drugs has surged.
Like any medical establishment in Gaza, GCMHCP faces a severe shortage of essential medications, forcing them to resort to alternatives. “We received the latest two batches of medication through WHO. But they are insufficient. In psychiatric treatment, it is preferable to continue with the same medication that has shown improvement, but unfortunately, we are forced to use alternatives that are not as effective,” Dr. Abu Obada explained.
The depletion of all types of psychiatric medications and the use of substitutes have negative effects on patients, including increased symptom severity, complications, and acute relapses. The two temporary bases have only been operating for four months, before which, many patients have discontinued their treatments, leading to severe relapses and complications.
Contact remains severed with many patients, and their fate remains unknown.
Accessing care in crisis
The difficult conditions patients face increase the suffering of their caregivers. Patients require containment and social support, especially those with psychotic disorders like schizophrenia. In the absence of medication and behavioral therapy, patients with such disorders experience severe nervous breakdowns, which can lead to self-harm and harm to others.
With families in overcrowded displacement areas along with inadequate societal awareness to handle such relapses, the load on caregivers to help and alleviate their patients’ suffering increases.
Meanwhile, families themselves undertake challenging daily tasks, requiring significant time and effort to provide basic necessities for their members, not to mention the intense psychological pressures they grapple with.
Dr. Abu Obada recounted the story of one such patient. “A woman wept to me: ‘My son hurt me, Doctor. He never did. My son has been off treatment for two months. I’ve been trying to contact anyone, but I couldn’t reach any.’” Dr. Abu Obada also explained how internet and communication cuts also contributed to contact being severed with a large number of patients, many of whom are now unaware of the new temporary locations and services.

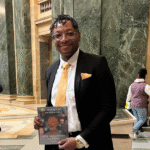
GAZA COMMUNITY MENTAL HEALTH PROGRAM STAFF PROVIDING PSYCHOLOGICAL SUPPORT TO DISPLACED CHILDREN, WOMEN, ELDERLY PEOPLE, AND PEOPLE WITH SPECIAL NEEDS IN EVACUATION CAMPS IN DEIR AL-BALAH AND RAFAH, IN APRIL 2024. (PHOTO: GAZA COMMUNITY MENTAL HEALTH PROGRAM/FACEBOOK)
Overcoming obstacles
One of the prominent services currently offered by the organization is the psychological first aid service (PFA). A trained team of psychologists conducts daily visits to various shelters, schools, camps, and displacement areas, reaching out to those in the darkest depths of despair, and offering a lifeline of psychological support.
Since most patients they deal with have experienced traumas, especially during the war, the team provides necessary first aid and refers those in immediate need of further intervention to the organization’s base for medication and behavioral therapy.
PFA team also provides group session therapy creating outlets for vulnerable sub-populations, like children, to help alleviate their feelings of fear, anxiety, grief, and anger.
Additionally, the team conducts awareness sessions to reduce the stigma associated with receiving mental health treatment.
“In March, PNGO Portal held a meeting for non-governmental organizations currently operating in Gaza under war conditions. We reinforced cooperation with other NGOs to facilitate referrals for cases in need of mental health care services,” Abu Obada explained.
GCMHP offers a toll-free line service at 1800 222 333. Specialists receive inquiries, provide consultations and teletherapy, and handle patient referrals. “In cooperation with our colleagues in the West Bank, staff from Ramallah answer inquiries from callers for 12 hours a day,” Dr. Abu Obada told Mondoweiss. Although the service has not been disturbed during the war, frequent communication blackouts have prevented its reach to service recipients.
As a non-profit organization dedicated to providing its treatments completely free of charge to its patients, GCMHP strives to secure funding affected by the lingering. “Our teams abroad are working hard to maintain support and facilitate delivering needed medications.”
As the aggression in Gaza persists, the dire state of mental health care exacerbates the suffering of its people. The absence of operational mental health centers in northern Gaza, coupled with the devastation of the only psychiatric hospital, leaves the population devoid of crucial support. The enduring trauma from years of aggression continues to strain the mental well-being of Gazans, underscoring the urgent need for sustained attention and resources to address this crisis amid the ongoing genocide.