Photo by Adobe Stock
This story comes to us from our partners at Feet in 2 Worlds, a project that brings the work of immigrant journalists to digital news sites and public radio.
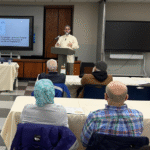
Mufti Mohammad Farhan juggles numerous responsibilities at the Islamic Center of Long Island in New York. On a Friday afternoon, he finishes leading prayers and departs for a funeral at the mosque. Since the pandemic, however, he has taken on a new role: identifying those in the Muslim community who need mental health support and referring them to clinical experts and therapists.
Across the United States, Muslim attitudes toward mental illness are changing, as is the role of the mosque. Following the COVID-19 pandemic, Muslims have been more willing to engage in public conversations regarding mental health issues, including the taboo subject of suicide. Imams and religious leaders have responded to worsening mental health problems in a variety of ways, including by taking mental health training. Although limited, such training can be a first step toward imams becoming a crucial part of the solution to their community’s mental health needs.
“We are often the first responders to mental health crises, because there is a trust factor that was built over time, and because of the huge stigma within our community,” explains Mufti Farhan, a soft-spoken religious leader who grew up in New York.
From a distance, the Islamic Center of Long Island on Brush Hollow Road appears more like a large complex of well-funded administrative offices and classrooms than a space for prayer. It is the oldest mosque on Long Island, accommodating up to 500 people, as well as shelter houses and a community pantry for those in need.
Farhan notes that since COVID-19, he has seen an uptick in stories of domestic violence and familial disputes whose most common theme is that the children of immigrants often express feelings of isolation and misunderstanding because of their bicultural identity.
Before and After the Pandemic: Mental Health in American Muslim Communities
“Many immigrant families think a mental health challenge can make their kids less suitable for marriage and acceptance, so they hide it or pretend it doesn’t exist,” explains Sayed Bhutan, a trainer with the Heal Collective.
According to the World Health Organization, global rates of anxiety and depression increased by 25% during the first year of the pandemic. In fact, in the United States, the percentage of adults who received treatment for their mental health over the preceding 12 months rose from 19.2% in 2019 to 20.3% in 2020 and 21.6% in 2021, according to a CDC report. White people were the most likely to receive mental health treatment; more than 30% of whites reported receiving mental health treatment in 2021, compared with 15% of Blacks, 13% of Hispanics, and 11% of Asians. As many foreign-born Muslims in the U.S. are Asian, and many U.S.-born Muslims are Black or Hispanic, the data suggests that Muslims receive lower levels of mental health treatment than their non-Muslim peers.
“COVID-19 opened the closed doors for Muslim Americans to speak out about their own mental health,” says Iman Farajallah, a psychologist who works with Muslim Arab-speaking clients struggling with addiction, domestic violence, and substance abuse in California. Despite a change in attitudes toward seeking help, high rates of poverty and unemployment in immigrant communities often make mental health treatment unaffordable. Other barriers include finding a therapist who understands immigrants’ religious or cultural backgrounds or the languages they speak.
When Farajallah surveyed 1,317 Muslim immigrants across the United States, almost half cited Arabic and Urdu as their primary spoken languages. “Unfortunately, there is a limited number of therapists able to communicate in different languages and understand the specific cultural and religious background of Muslim Arabic- or Urdu-speaking communities,” Farajallah explains.
Sarah Murad, a counselor at the Islamic Circle of North America’s humanitarian arm, has been providing culturally competent care to immigrant communities in Illinois, a state with the highest per-capita population of American Muslims in the U.S., many of whom are religious conservatives or recent immigrants. “By the time people come to seek our help, it is already too late because of the stigma [around mental health], so the first thing they ask for is a religious counselor,” Murad says. In such instances, she refers cases to Shaykh Omer Haqqani, who works at the Islamic Center of Wheaton and provides culturally relevant therapy and khutbahs, or sermons, about mental health across Illinois.
“Our faith tells us that it’s OK to be sad and express our emotions,” says Haqqani. He often cites the following story to those who seek his help: “When our prophet Muhammad (PBUH) lost his infant child—he was weeping, he was mourning, he was crying to the point where the companions came and asked him, ‘Even you, the prophet of God?’”
The causes of mental health issues among Muslim Americans have been linked to increased Islamophobia since the 9/11 attacks. Psychology professor Amy Weisman de Mamani of the Muslim American Project at the University of Miami uses research to raise awareness about the unique psychological needs of Muslim American communities. She says Islamophobia as well as bias in therapy and society can make Muslim Americans vulnerable to what psychologists call “thwarted belongingness” and “perceived burdensomeness,” two risk factors for depression and suicide behavior.
“Because there is much Islamophobia and fear since 9/11, if somebody is distressed, they would be less likely to want to go and talk to a therapist. Even if they’re not worried about being reported, they’re worried about how they’re going to be perceived,” Weisman explains.
For religious leaders, like Haqqani in Illinois and Farhan on Long Island, the shift toward seeking mental health care is happening at Islamic centers and mosques. Both men cite an expansion of the role Islamic centers play in the lives of community members. “For Muslims, one of the most important and effective venues to get information about mental health is at the mosque, and topics such as suicide and depression are now openly being addressed in khutbahs,” Haqqani shares.
How One Specific Study Triggered Backlash—And a Push for Action
In April 2021, a study in the Journal of the American Medical Association (JAMA) showed that nearly 8% of Muslim adults reported a suicide attempt in their lifetime—compared with 6% of Catholics, 5% of Protestants, and 3.6% of Jewish respondents. This pre-pandemic study sparked a backlash within traditional religious circles, with one scholar tweeting that the study was inaccurate. Daniel Haqiqatjou, an anti-feminist conservative Islamic commentator, wrote that the research is “unethical” and part of a campaign to push “liberal policies” and cast a negative light on American Muslims and Islam.
Despite this backlash, the authors stand by their findings. “What we have seen clinically and anecdotally is now proven,” says Rania Awaad, a director of the Muslim Mental Health & Islamic Psychology Lab at Stanford University and one of the study’s authors. She adds, “There is an increase in suicide attempts in Muslim American communities, [to] which especially our imams used to say, ‘No, no, no, this is not an issue.’”
Awaad recalls a specific incident in Texas that became a turning point for religious leaders seeking help in addressing mental health needs. In April 2021, six people were fatally shot in a suburban Dallas home after two Muslim brothers with a history of mental illness made a pact to kill their family members and die by suicide. Within 24 hours, Awaad was leading an emergency training via Zoom with a group of imams in Dallas who had turned to her for help.
From this experience, Awaad noticed how religious leaders tend to ask for intervention only after a crisis has occurred, and together with her team at Stanford University, she launched a campaign to train 500 Muslim leaders on suicide response.
Amara Kamara, a 53-year-old first-generation immigrant from Liberia, attended Awaad’s training in his capacity as a mental health advocate and administrator at Masjid Al-Ansar in Minnesota. He saw it as a “new experience” that allows him to “see how we can use community resources to have an open discussion about a difficult topic and tell the victims that it is OK to talk about it.”
The Future of Muslim American Mental Health
Muslim Americans are racially diverse, and 75% are immigrants or the children of immigrants. Amelia Noor-Oshio is the first self-identifying Muslim American to receive federal funding from the National Institutes of Health to conduct grassroots mental health research within this community. For her, structural oppression and Islamophobia are at the heart of stigmas against mental health care, on par with social and political pressures. She finds, “Muslim mental health is about social equity, accessibility, and the reality of living a minoritized experience and with [a] stigmatized identity where you don’t have as much power and protection as someone who is white, straight, able, neurotypical, and heterosexual.”
Beyond structural issues, there are other community-specific barriers to mental health facing the Muslim community. Two Muslim social workers who did not want to be identified share that they recently worked with eight clients who had suicidal thoughts. Those clients had easy access to handguns, and their gender identity was changing in ways that their parents did not accept.
“It’s gun access, social and political divisions, mass shootings becoming normal, then the stigma,” one of them explains. “So, if you live in an isolated suburb, have no mosque or Islamic center that welcomes you as you are, the risk factors will be more substantial and enduring.”
Shaheen Ahmad, co-founder of the Muslim American Project at Miami University, provides culturally informed, spiritually integrated mental health care to Muslims in Florida. Looking to the future of mental health access, he sees the Muslim community as increasingly open to recognizing new and old mental health problems, saying, “We have more collaboration and conversations between mental health professionals and religious leaders than 10 or 15 years ago.”
To back up his optimism, he explains, “We have more community centers and more open spaces. We have more people who are doing scientific research and culturally-informed therapy, and who care about combining … the two.”
By Majd Al-Waheidi