© Photo
Mouna Photography for the Wisconsin Muslim Journal
Rehab for stroke patients and those suffering from spinal cord injuries is about to take a great leap forward with the aid of 21st century robotics, and a UWM researcher is at the forefront of this change.
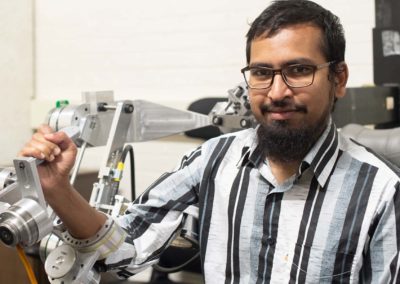
Assistant professor Mohammad Habib Rahman of the mechanical and biomedical engineering departments is a pioneer in a new field of robotics that has the potential to revolutionize physical therapy.
These assistive technologies won’t replace the work of therapists. Instead, they will help patients work longer and harder, often from their own homes, in doing the specialized work that physical therapists have assigned for them.
As Professor Rahman explains, “Exoskeleton robotics, a relatively new kind of assistive technology, involves wearable frameworks that cover the surface of limbs and boost injured muscles’ electrical impulses” – something like Iron Man’s amazing flight suit, but tailored specifically to a non-functioning body part.
Rahman and his team are designing for people whose limbs are paralyzed or who have “spasticity” as the result of cerebrovascular accident (stroke), spinal cord injury, occupational injury, and/or orthopedic injury. “When people suffer a cerebrovascular accident, the affected area of the brain loses its ability to send motor commands to the peripheral nervous system, which is responsible for driving the musculoskeletal system. In course of time, the brain forgets to command/perform even a simple movement such as a hand movement. The patient has no control,” says Rahman, and is not able to perform ordinary motor functions. The purpose of physical therapy is to help the brain relearn those motor functions
But in this case, “The robot will stretch you,” Rahman says. “The idea is to mimic the therapist. It’s a form of passive, active, and active-assisted rehabilitation therapy. It does the boring task for the therapist.”
The exoskeleton contains “electrodes on the skin [that] detect human intention of movement when the patient’s limbs are getting only a weak signal from the brain,” says Dr. Rahman. The electrodes “know” the patient’s intention from muscle signals. Then the exoskeleton enables the movement as needed.
This process is one of “teaching the brain the repetitive motions” of the muscles, just as working with a physical therapist does. But the AI-equipped exoskeleton “can do the task for a longer period of time than the therapist” says Rahman. This “helps to build back muscle tone and reconnect the brain signal.”
Rahman says he and his team are only a few months from completing the latest version of whole-arm assistive technology. (A robotic glove that will assist finger motion is still in the prototype phase.) With a $50,000 grant through the National Science Foundation I-Corps Program, they are working on customer discovery and developing a business model. “Customer discovery helps modify product,” he says.

Currently, the team working under the I-Corps grant includes senior scientist Rathindra DasGupta, doctoral student Md Assad Uz-Zaman, and undergraduate Fidel Sierra-Flores, Jr.
Rahman’s game plan is to “open a start-up with my students,” while teaching them about entrepreneurship and innovation. “I want to solve the problems that can benefit society,” he says. “You want something that has really impacted society.
Dr. Rahman began his career in robotics in 2003 at Saga University in Japan before entering the PhD program at the University of Quebec, where he opened the bio-robotics lab. The Japanese are “the boss in robotics,” he says.
In Japan, he worked on a wheelchair-mounted robot to help weak or elderly people with routine tasks. His team at UWM is now working on the second phase of this project. The new wheelchair mounted robotic exoskeleton will be able to provide both rehabilitation therapy and activities of daily living assistance at the level of shoulder, elbow, and wrist joint movements. Like the exoskeleton, it “will align with your own powers and detect your signals,” Rahman says. “If we can make a low-cost device, wheelchair mounted. . . insurance can cover [it].”
Rahman and his team are partnering with the VA in designing and testing the robotic, wheelchair mounted, multi-functional assistive arm that aims to make those with spinal cord injuries more independent, to help them “go outside, pick up objects, eat. The robot has a magazine of grippers attached to is base” that will help patients perform these basic tasks, Dr. Rahman says.
A key element of his current research is how to make devices smarter by connecting them to the Cloud so that patients are able to remain home-based rather than needing to move into nursing homes. “If we can make [the device] mobile, the doctor can remotely prescribe activity and remotely advise” the patient, Rahman says.
“Travel is another problem,” he says. Today, wheelchair-bound patients are reliant on others to take them to the hospital or to rehab, and this, says Rahman, results in many “dropouts from rehab.” But the new devices, including the robotic glove that will assist stroke patients with finger motion, will largely eliminate the need to travel elsewhere for treatment, replacing it with customized “home-based rehab care.”
Another of Rahman’s projects is a Wisconsin Space Consortium grant for “adaptive coordination control of multiple mobile manipulator robots” that will help NASA land teams on Mars.
A key part of his team are the nine PhD students Rahman currently supervises. One PhD and three ME students have graduated from his lab, and more than 35 undergraduates have researched in his lab in the four and a half years he has been at UWM. “My students work really hard, late into the night. I’m really proud of them,” Professor Rahman says.